
Introduction
Safe sex is a critical aspect of sexual health, focusing on reducing the risks of sexually transmitted infections (STIs), unintended pregnancies, and emotional strain. By adopting safe sex practices, individuals can enjoy a healthy and fulfilling sexual life while ensuring protection for themselves and their partners. This guide delves into various safe sex practices, offering insights to help individuals make well-informed decisions. Practicing safe sex promotes overall health and well-being by reducing exposure to STIs such as HIV, gonorrhea, chlamydia, and syphilis. Additionally, it prevents unintended pregnancies, giving individuals greater control over family planning and reproductive choices.
Beyond the physical benefits, safe sex nurtures trust and communication in relationships. Open discussions about protection and boundaries strengthen emotional connections and foster mutual respect. They also normalize conversations about consent, sexual health, and personal comfort, contributing to healthier relationships.
Safe sex empowers individuals to make educated choices, alleviates anxiety, and promotes confidence in intimacy. Prioritizing these practices is essential for fostering physical, emotional, and relational well-being.
1. The Importance of Safe Sex
Practicing safe sex helps prevent STIs, including HIV, chlamydia, gonorrhea, syphilis, and human papillomavirus (HPV). It also minimizes the risk of unintended pregnancies and fosters healthy communication and trust, allowing boundaries and preferences to be respected.
2. Communication and Consent of Safe Sex
Open communication and mutual consent form the foundation of safe sex.
Open Dialogue for safe sex: Discuss sexual history, STI testing, contraceptive use, and boundaries before sexual activity. Transparency can ease anxiety and foster trust.
Informed Consent for safe sex: Both partners must enthusiastically agree to any sexual activity. Consent should be ongoing and revocable at any time, relying on verbal and non-verbal cues.
Respect Boundaries for safe sex: Always honor personal boundaries. Respecting limits strengthens relationship dynamics.
Pros:
- Builds trust and transparency
- Reduces misunderstandings
- Ensures comfort and safety
Cons:
- Initial discomfort or awkwardness for some
- Miscommunication without proper skills
3. Barrier Methods

Barrier methods of birth control are designed to physically prevent sperm from reaching the egg, thereby preventing fertilization. These methods are typically used before or during intercourse and include male and female condoms, diaphragms, cervical caps, and contraceptive sponges. As a non-hormonal option, they can also help reduce the risk of sexually transmitted infections (STIs), particularly when condoms are used. They are effective at preventing pregnancy and reducing the transmission of sexually transmitted infections (STIs).
Male Condoms: Made from latex, polyurethane, or polyisoprene, : A protective cover placed over the penis during intercourse to block the release of semen into the vagina, anus, or mouth. They are easy to use and accessible.
Female Condoms: Inserted into the vagina or anus before intercourse, they offer an alternative for those with latex allergies.
Dental Dams: Thin latex sheets used during oral sex to prevent STI transmission. They can be made from cut-open condoms or purchased commercially.
Effectiveness: Properly used, condoms effectively prevent STIs and reduce pregnancy risk.
Diaphragms: Flexible, dome-shaped silicone barriers placed over the cervix to prevent sperm from reaching the uterus. They should be used with spermicide for optimal effectiveness.
Cervical Caps: Similar to diaphragms but smaller, cervical caps are inserted over the cervix and used with spermicide for enhanced pregnancy prevention.
Pros:
- High STI protection
- Widely available and affordable
- Minimal side effects
Cons:
- Potential reduced sensitivity
- Risk of breakage or slippage
- Latex allergies in some individuals
4. Hormonal Contraceptives
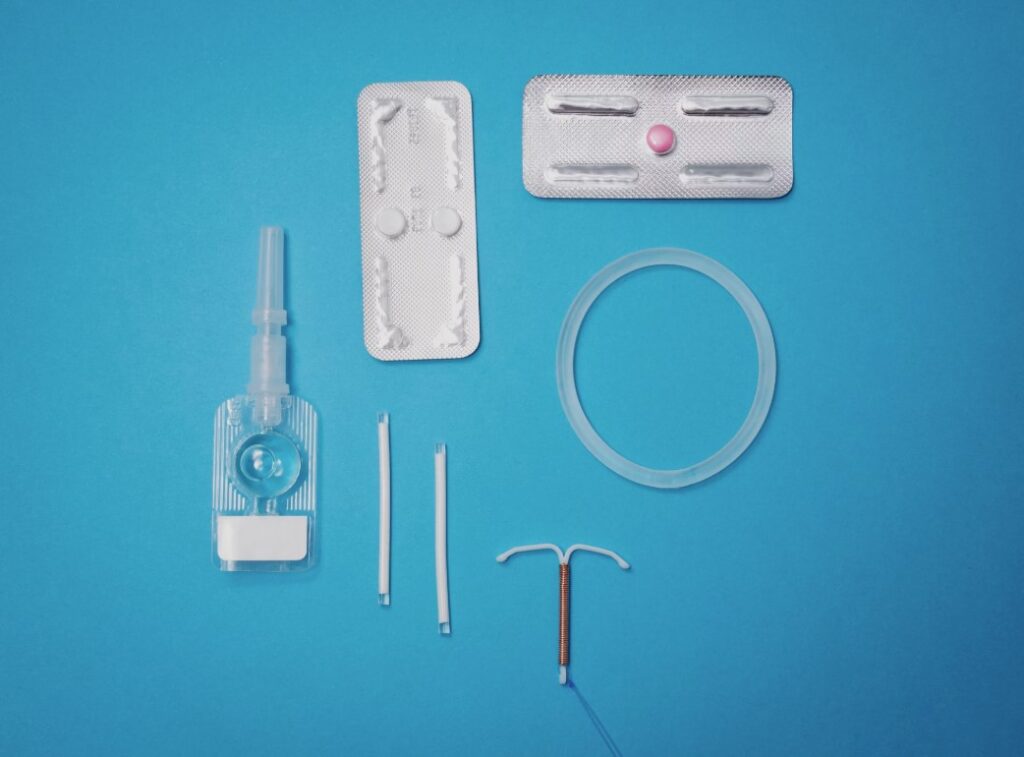
Hormonal birth control methods use estrogen, progestin, or a combination of both to prevent pregnancy. They work by inhibiting ovulation (the release of an egg from the ovary), thickening cervical mucus to block sperm, and thinning the uterine lining to prevent implantation of a fertilized egg. Hormonal contraceptives prevent pregnancy by regulating ovulation but do not protect against STIs. These methods are widely used and are available in various forms, including:
Birth Control Pills: Daily pills containing hormones to prevent ovulation, also useful for menstrual cycle regulation.
Injections: Administered every few months to prevent pregnancy.
Patches: Worn on the skin, these release hormones to inhibit ovulation.
Implants: Hormone-releasing rods inserted under the skin for long-term use.
Vaginal Rings: Flexible rings inserted into the vagina to release hormones over a set duration.
Pros:
- Highly effective for pregnancy prevention
- Convenient for regular use
- Can regulate cycles and ease cramps
Cons:
- No STI protection
- Potential side effects like mood changes or nausea
- Requires adherence to schedules
5. Long-Acting Reversible Contraceptives (LARCs)
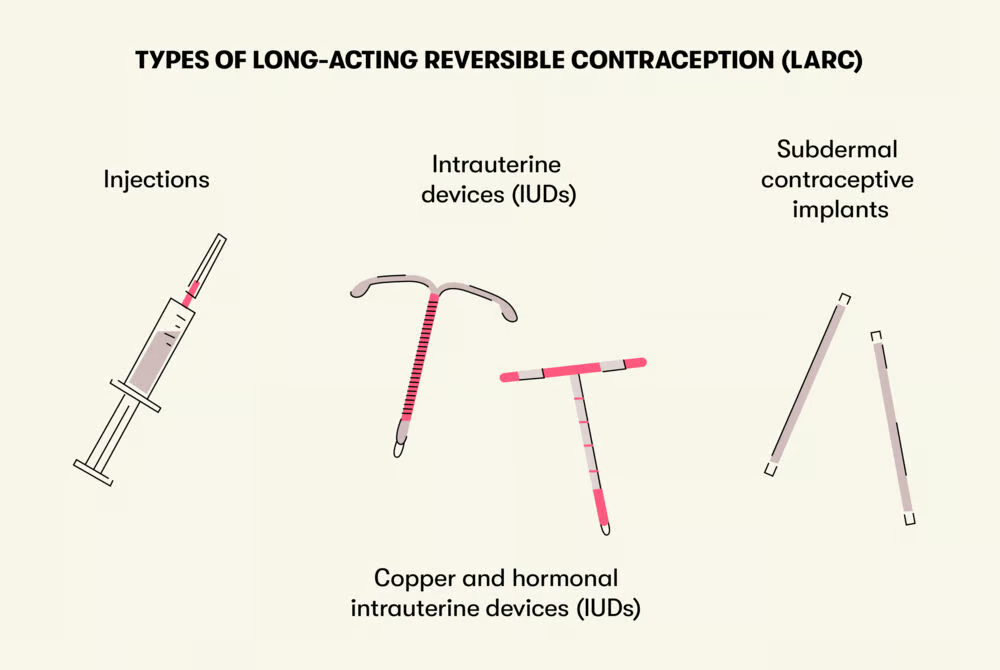
LARCs, or Long-Acting Reversible Contraceptives, are methods of birth control that provide extended protection against pregnancy and can be discontinued at any time, with fertility returning rapidly. These options, such as IUDs and implants, are popular for their long-lasting effectiveness and ease of use. LARCs offer long-term contraception without daily maintenance.
Intrauterine Devices (IUDs): Small T-shaped devices inserted into the uterus. Hormonal IUDs release progestin, while copper IUDs deter sperm.
Effectiveness: LARCs are highly effective with low failure rates.
Pros:
- Long-lasting protection (3-10 years)
- Minimal maintenance
- Highly effective
Cons:
- Discomfort during insertion
- No STI protection
- Rare risks of expulsion or complications

Emergency contraception is a backup method to prevent pregnancy after unprotected intercourse or contraceptive failure, such as a broken condom or a missed birth control pill. It is designed for occasional use, not as a regular contraceptive method, to reduce the likelihood of unintended pregnancy. There are two primary types of emergency contraception:
Morning-After Pills: Over-the-counter pills most effective within 72 hours of unprotected intercourse.
Copper IUD: Inserted within five days of unprotected sex to prevent pregnancy.
Pros:
- Effective post-exposure pregnancy prevention
- Easily accessible
Cons:
- Less effective than regular contraceptives
- No STI protection
- Potential side effects like nausea

Regular STI testing is crucial for maintaining sexual health.
STI testing and treatment involves detecting and managing sexually transmitted infections (STIs). Testing typically includes blood tests, urine samples, or swabs to check for infections like chlamydia, gonorrhea, HIV, and syphilis. If an STI is detected, bacterial infections are treated with antibiotics, while antiviral medications help manage viral infections. Regular testing and prompt treatment are crucial for maintaining sexual health and preventing the spread of STIs.
The process of STI testing and treatment helps identify and address sexually transmitted infections. Testing can be done using blood, urine, or swab samples to screen for infections such as HIV, gonorrhea, and syphilis. Treatment varies depending on the infection type—antibiotics are used for bacterial infections, while antivirals help manage viral STIs. Regular screening and early treatment are key to promoting sexual well-being and reducing transmission risks.
Routine Testing: Get tested before new relationships and at regular intervals.
Partner Testing: Encourage partners to get tested and share results.
Treatment: Prompt medical attention for STIs prevents complications. Many STIs are treatable with early intervention.
Pros:
- Early detection prevents complications
- Reduces transmission risks
Cons:
- Potential discomfort during tests
- Social stigma may deter testing
8. PrEP and PEP

PrEP and PEP are medications to prevent HIV.
PrEP: Daily medication that reduces HIV risk, recommended for high-risk individuals.
PEP: A 28-day medication course taken within 72 hours of potential HIV exposure.
Pros:
- Highly effective for HIV prevention
Cons:
- Requires strict adherence
- Potential side effects like fatigue

Abstinence: Complete avoidance of sexual activity ensures no STI or pregnancy risks.
Monogamy: Exclusive relationships with STI-free partners reduce infection risks.
Pros:
- No STI or pregnancy risks (abstinence)
- Builds trust and intimacy (monogamy)
Cons:
- Abstinence may not be sustainable for everyone
- Monogamy relies on mutual trust
10. HPV Vaccination
HPV is a common STI linked to various cancers.
Vaccination: Recommended for individuals aged 9-26, with potential benefits for adults up to 45.
Effectiveness: Protects against common cancer-causing HPV strains.
Pros:
- Prevents HPV-related cancers
- Safe and well-tolerated
Cons:
- Limited strain coverage
- Requires multiple doses
Proper hygiene reduces infection risks.
Washing Genital Areas: Clean before and after sex to reduce bacteria.
Urination: Urinating post-sex flushes out bacteria.
Avoid Douching: Douching disrupts bacterial balance and increases infection risks.
Pros:
- Reduces bacterial infections
- Accessible and easy
Cons:
- Over-washing may irritate
12. Managing Multiple Partners
Precautions are essential for those with multiple partners.
Consistent Condom Use: Use condoms or dental dams with new partners.
Regular Testing: Frequent STI tests ensure early detection.
Open Communication: Be honest about sexual history and testing.
Pros:
- Reduces STI risks
- Promotes responsibility
Cons:
- Requires vigilance
- Potential emotional complexities
13. Mental and Emotional Well-Being
Mental health is crucial in safe sex practices.
Avoid Coercion: Do not engage in sexual activity under pressure.
Emotional Readiness: Ensure emotional preparedness to prevent regret or anxiety.
Seek Support: Consult counselors for sexual anxiety or trauma.
Pros:
- Promotes healthy relationships
- Reduces stress
Cons:
- Requires self-awareness
14. Educating Yourself and Others
Education is key to safe sex.
Resources: Utilize reputable websites, clinics, and healthcare providers.
Community Support: Join groups discussing sexual health.
Peer Education: Share knowledge about safe sex practices.
Pros:
- Empowers individuals
- Fosters healthy communities
Cons:
- Misinformation risks
Conclusion
Safe sex is a shared responsibility involving communication, protection, regular testing, and mental well-being. Comprehensive practices safeguard physical and emotional health while fostering fulfilling relationships. By prioritizing education, barrier methods, vaccinations, and open communication, individuals can take charge of their sexual health. Embracing these practices enhances trust, intimacy, and respect, ensuring positive and safe experiences for all.
Recommend:
The Role of Parents in Sex Education 101: How to Guide Your Child Towards Healthy Sexual Awareness
The Fundamentals of Sex Education 101: Importance, Topics, and Global Perspectives
https://en.wikipedia.org/wiki/Safe_sex
https://en.wikipedia.org/?title=Safe-sex&redirect=no
